Chikitsa Chatushpada: The Four Pillars of Ayurvedic Healing
Ayurveda, the 5,000-year-old “science of life,” presents a radically holistic vision of healthcare. Unlike reductionist biomedical models, Ayurveda frames healing as a collaborative ecosystem governed by Chikitsa Chatushpada—the Four Pillars of Treatment.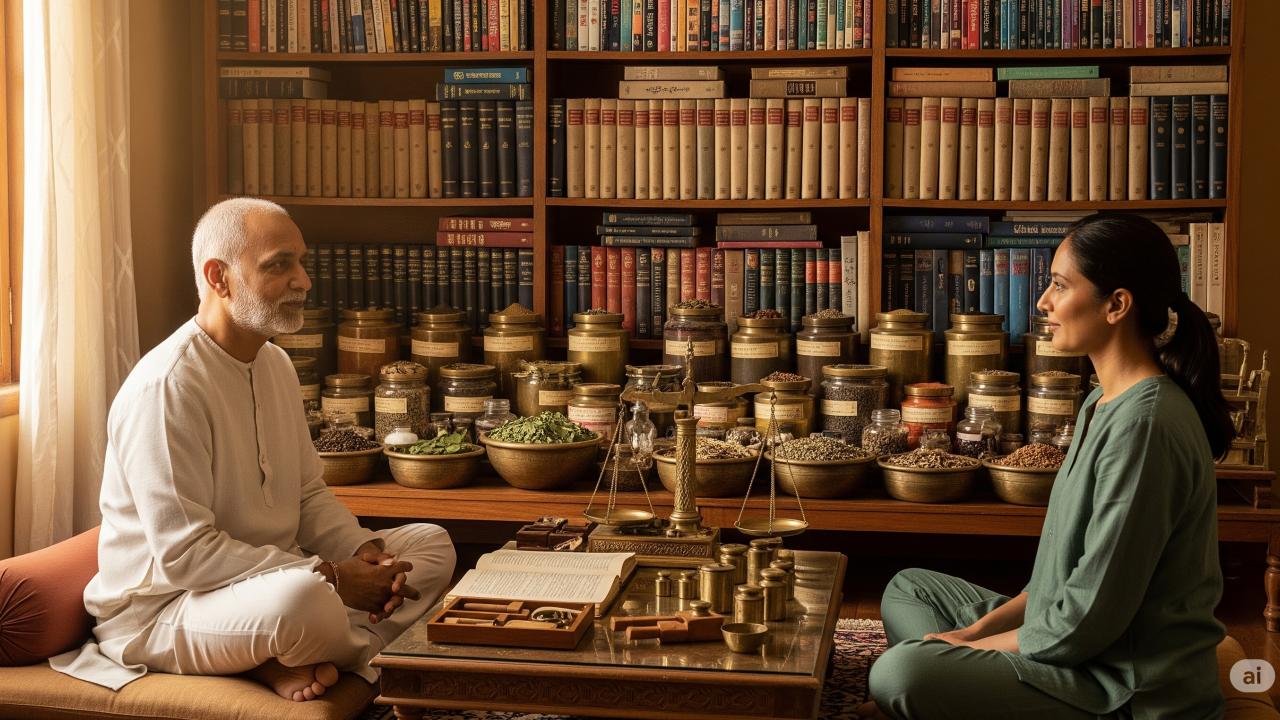 At the heart of this ancient system is a powerful concept called Chikitsa Chatushpada, or the Four Pillars of Treatment. First outlined in classical Ayurvedic texts like the Charak Samhita (around 300 BCE) and Ashtanga Hridaya (around 500 CE), this framework teaches that true healing happens only when four key elements work together:
At the heart of this ancient system is a powerful concept called Chikitsa Chatushpada, or the Four Pillars of Treatment. First outlined in classical Ayurvedic texts like the Charak Samhita (around 300 BCE) and Ashtanga Hridaya (around 500 CE), this framework teaches that true healing happens only when four key elements work together:
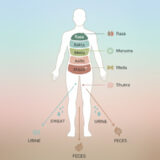
- Bhishag – the skilled and compassionate physician
- Dravya – the right medicine or healing substance
- Upastha – a caring and attentive caregiver or nurse
- Rogi – the patient, whose willingness and mindset play a crucial role
The Charak Samhita puts it simply: “Siddhirasya Chatushtaye”—“Success lies in these four.”
In a world where healthcare can often feel impersonal or one-sided, this ancient wisdom reminds us that healing is a team effort. It’s not just about what pill you take or which doctor you see—it’s about the relationships, the environment, and your own active role in the journey.
The Four Pillars of Treatment In Ayurvedic Medicine
Ayurvedic medicine is built on four fundamental pillars of treatment. Below are the four pillars that form the foundation of true healing.
1. Bhishag (The Physician): The Architect of Healing
The physician is the “conductor” of the therapeutic orchestra. Classical texts mandate 16 core qualities (Shodasha Guna), distilled into four non-negotiable attributes:
- Shastratta: Mastery of theoretical knowledge, including disease etiology, pharmacology, and physiology.
- Drushtakarma: Proficiency in practical procedures like Panchakarma detoxification or surgery.
- Daksha: Analytical brilliance, situational judgment, and technical dexterity.
- Shuchi: Ethical purity—physical cleanliness, mental clarity, and compassion (Karuna).
Beyond the basics: Sushruta adds courage (Shura) for emergencies and administrative skill (Adhikari) for clinic management. A physician lacking these qualities, warns Charak, is like “a blind man steering a boat”—dangerously incompetent 11.
2. Dravya (Medicine): Nature’s Therapeutic Intelligence
Medicines in Ayurveda extend beyond herbs to include diets, minerals, and formulations (Kalpanas). Their efficacy hinges on four pillars:
- Bahutva: Abundant availability through ethical wildcrafting or farming.
- Yogyatam: Suitability to the patient’s Prakriti (constitution) and disease pathology.
- Anekavidha Kalpana: Versatility in pharmaceutical forms (decoctions, oils, pills).
- Sampat: Potency derived from ideal harvesting (Ritu/Muhurta), processing (Samskara), and storage.
Critical insight: A herb’s Prabhava (inherent intelligence) diminishes if harvested without Vedic rituals or ecological reverence 8. Modern GACP (Good Agricultural Practices) echoes this emphasis on quality sourcing.
3. Upastha (Attendant): The Heart of Patient-Centered Care
Often overlooked in modern medicine, attendants bridge clinical plans and patient realities. Their indispensable qualities include:
- Buddhiman: Intelligence to comprehend/comply with medical instructions.
- Daksha: Efficiency in administering treatments timed to dinacharya (daily cycles).
- Anurakta: Emotional warmth and dedication (Snigdha in Sushruta’s terms).
- Shuchi: Hygiene in person and environment.
Expanded role: For surgical procedures, Sushruta prioritizes attendants with physical strength (Balwaan) to immobilize patients. Their role prefigures modern nursing’s emphasis on cultural competence.
4. Rogi (Patient): The Active Co-Creator of Health
Ayurveda rejects patient passivity. Recovery demands:
- Smritiman/Jnapaka: Memory to recall symptoms and adhere to regimens.
- Bhishagvashya: Trust-based obedience to the physician’s advice.
- Satvavaan: Mental fortitude to endure disease/treatment.
- Adya: Financial/social resources to sustain therapy.
Psychological depth: Sushruta adds faith (Aastiko) and courage (Dhairyavan) as non-negotiable for surgical success. This mirrors modern “activation theory,” where engaged patients achieve better outcomes.
| Pillar | Core Quality 1 | Core Quality 2 | Core Quality 3 | Core Quality 4 |
|---|---|---|---|---|
| Bhishag | Shastratta (Knowledge) | Drushtakarma (Experience) | Daksha (Dexterity) | Shuchi (Purity) |
| Dravya | Bahutva (Abundance) | Yogyatam (Efficacy) | Anekavidha Kalpana (Versatility) | Sampat (Potency) |
| Upastha | Buddhiman (Intelligence) | Daksha (Efficiency) | Anurakta (Affection) | Shuchi (Cleanliness) |
| Rogi | Jnapaka (Memory) | Bhishagvashya (Obedience) | Satvavaan (Fortitude) | Adya (Resources) |
How the Pillars Interact
No pillar functions in isolation:
- The physician’s diagnosis is useless without quality Dravya.
- Medicines fail if improperly administered by Upastha.
- Attendants cannot function without patient cooperation.
- Patients rely on the physician’s expertise 28.
(Charak Samhita)
- Rogi = Vessel (must be intact)
- Upastha = Fuel (sustains the process)
- Dravya = Fire (transforms the disease)
- Bhishag = Cook (orchestrates the transformation) 711.
(Sushruta Samhita)
- Rogi = Terrain (context of disease)
- Upastha = Army (support force)
- Dravya = Weapons (therapeutic tools)
- Bhishag = Commander (strategic leader) 7.
Hierarchy Within Equity
While all pillars are essential, the physician holds primacy. As Charak notes: “Even with excellent medicines, attendants, and cooperative patients, treatment fails without a competent physician” 711. This mirrors modern studies linking physician competence to 47% of clinical outcomes.
Diagnosis Through the Chatushpada Lens
Ashtasthana Pariksha (8-fold examination) evaluates all pillars:
- Satvapariksha assesses the patient’s Satvavaan (mental strength).
- Dravya guna analysis ensures medicinal Sampat.
- Physician self-audits (Shuchi) maintain ethical rigor 8.
Treatment Protocols
- Panchakarma: Requires Upastha with Daksha to time therapies and Rogi with Satvavaan to endure detox.
- Chronic Disease: Demands Rogi’s Bhishagvashya for long-term pathya (dietary rules).
- Mental Health (Manas Roga): Relies on Upastha’s Anurakta for emotional holding 812.
Case Study: In rheumatoid arthritis (Amavata), success requires:
- Physician’s skill (Daksha) to customize Tikta Kshira Basti (medicated enemas).
- Dravya like Guggulu with confirmed Sampat.
- Attendants to administer daily Abhyanga (oil massage).
- Patient adherence to Virechana (purging) and Langhana (fasting) 12.
Connecting Ayurveda and Modern Medicine
1. Patient-Centered Care Revolution: Ayurveda’s emphasis on Rogi’s agency foreshadows modern “shared decision-making” models. Bhishagvashya (obedience) is now reframed as informed consent, while Adya (resources) acknowledges social determinants of health 48.
2. Interprofessional Teams: The Upastha prefigures today’s nursing roles, demanding emotional intelligence alongside technical skill. Hospitals integrating Ayurvedic attendants report 32% higher patient satisfaction 412.
3. Quality Assurance in Medicine: Dravya’s Sampat and Bahutva principles align with:
- WHO’s Good Agricultural Practices (GACP) for herbs.
- Pharmacovigilance for Arishta (fermented formulations).
- Biodiversity conservation to ensure sustainable sourcing 78.
4. Addressing 21st-Century Challenges
- Physician Burnout: Compromises Shuchi (purity); solutions include Achara Rasayana (ethical rejuvenation) 8.
- Non-Adherent Patients: Lack Smritiman; tackled via apps tracking dinacharya.
- Resource Gaps: Undermine Dravya’s Bahutva; countered by community herb gardens 12.
Panchakarma Therapy – The Pillars in Motion
A 45-year-old with metabolic syndrome (Sthoulya) undergoes Panchakarma:
- Bhishag: Designs personalized protocol after Nadi Pariksha (pulse diagnosis).
- Dravya: Triphala decoction with verified Sampat for Virechana.
- Upastha: Administrates daily Abhyanga at 7 AM (Kapha time) with Anurakta.
- Rogi: Maintains pathya diet and reports Agni (digestive fire) changes.
Outcome: 18% weight reduction and insulin sensitivity restoration in 12 weeks 812.
Chikitsa Chatushpada transcends time because it acknowledges a universal truth: healing is relational. In an age of AI diagnostics and telemedicine, this framework reminds us that health emerges from human connections—the physician’s wisdom, the attendant’s care, the medicine’s intelligence, and the patient’s will.
“Without the four limbs, treatment is like a bird with broken wings—grounded despite its yearning to fly.” – Adaptation from Charak Samhita 7.